Wear a mask - it's airborne!
Table of Contents
- N95, FFP2, KF94, KN95 and CN95
- We knew from the start that masks would help slow or stop even the pandemic
- Pre-pandemic articles
- Articles written during the pandemic
- Goddard’s Journal - listing the “masks work” studies
- Scientific studies of masks and respirators
- Systematic and meta-analyses of masks and respirators
- Actual studies (not meta-analyses)
- Narrative reviews
- Anti-masker activities
Until ventilation laws are enacted and building owners roll out change to increase fresh air, HEPA/MERV filter stale air and use CO2 monitors to gauge proximate transmission risks, your only way to be confident about protecting yourself inside shard-air spaces is to wear a mask. We realize that most people in 2024 are not wearing masks for protection at all. Understand that a few people still are, and that they ignore the comments they get.
There were lies about masks and respirators from the start of the pandemic. Ignore them, all masks work, but they vary from 10% protective up to 99.9%. Here’s the definitive study: Masks and respirators for prevention of respiratory infections: a state of the science review - Greenhalgh et al, 2024.
- If you are in a country that has some circulation of Covid-19, maybe wear a mask when mixing with others in enclosed spaces, whether you or others are vaccinated or not.
- We’re long past the era where simple cloth masks are good enough.
- If you can afford N95, FFP2, KF94 respirators then consider having those. If you’re careful taking them off and putting them on, each can last many tens of hours.
The difference between N95, FFP2, KF94, KN95 and CN95
If you can afford it, get N95/KF94 grade masks (that are not cloth or washable) for use when mixing with other in public. Citizen Scientist, Aaron Collins, reviews masks for filtration effectiveness and talks about KF94 masks quite a bit, but there are many standards now.
From the fall of 2020 onwards, Aaron Collins with the equipment he had at his home tests high-filtration masks he’s acquired for filtration and leakage. One of the stars of “masks for all” in the pandemic.
We knew from the start that masks would help slow or even stop the pandemic.
Pre-pandemic articles suggesting masks in particular would work
- 2008: UK’s Health and Safety Executive identifies surgical masks as protective on some basis. UK’s FFP2 would have been much better, but at least it doesn’t say “masks are bad”. Surfaced at the start of the pandemic by Tom Andrews
Here are some articles written during the pandemic supporting the use of masks
- March 25, 2020; Goddard’s Journal video: first review of mask studies over the years and that they work
- May, 2020: University of Chicago and Argonne National Labs (USA): Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks - Konda et al.
- October 15, 2020; Goddard’s Journal video: second review of mask studies over the years and that they work
- Since March 2020; damerousky.cz: Citizen made portal for making masks, started in the Czech Republic (Europe) and now an international multi-language effort
- Active since March 2020; Masks4all.co portal has been pushing the “masks for all” message. And a discussion forum on reddit for the same
- Masks do not create a false sense of security, See Twitter thread by Rob Shirkey
- Aug, 2020: Max-Planck Institute (Germany): Aerosol filtration efficiency of household materials for homemade face masks: Influence of material properties, particle size, particle electrical charge, face velocity, and leaks - Drewnick et al.
- August, 2020; Webmd article: Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US
- August 26, 2020; Wei Lyu and George L. Wehby study: The Forgotten Science Behind Face Masks
- Nov, 2020: Virginia Tech: Cloth face coverings help protect both wearers and those nearby - Pan, Harb, Leng & Marr.
- December 2020; William G. Lindsley: Efficacy of face masks, neck gaiters and face shields for reducing the expulsion of simulated cough-generated aerosols
- Dec, 2020: University of Wisconsin “fitter” study (see fitters)
- January 26, 2021; Jeremy Howard et al: An evidence review of face masks against COVID-19
- January 27, 2021; Slate e-Zine: Do You Really Need Two Masks Now?
- January 28, 2021; Salon e-Zine: How high-filtration masks — like the KN95, N95 and KN94 — differ
- January 28, 2021; CBC: Why you might want to start wearing better masks — even outdoors
- January 28, 2021; Buzzfeed: What Is Double-Masking? Here’s How It Can Keep You Safer From The Coronavirus
- January 29, 2021; New York Times & Colorado State Mask Study: How to Choose the Best Cloth Face Mask for You
- Feb, 2021: Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2 - Brooks & Butler
- March 5, 2021; The Virus Spread Where Restaurants Reopened or Mask Mandates Were Absent
- Apr, 2021;The Impact of Universal Mask Use on SARS-COV-2 in Victoria, Australia on the Epidemic Trajectory of COVID-19
- May, 2021: Cheng, Ma2, Witt, Rapp, Wild, Andreae, Pöschl, and Su: Face masks effectively limit the probability of SARS-CoV-2 transmission
- June 5, 2021; Cheng et al: Face masks effectively limit the probability of SARS-CoV-2 transmission
- June 29, 2021; BBC: Covid: Masks upgrade cuts infection risk
- July 21, 2021; Scott et al: The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in a major metropolitan city
- July 22, 2021; Study reveals mask rule turned Melbourne’s deadly second wave ‘overnight’ Studu itself.
- Aug 6 2021; “Wearing a mask is not a political statement”
- Aug 19, 2021; Study supports widespread use of better masks to curb COVID-19 indoors
Wikipedia Maintains a long page on mask use in the pandemic here
Goddard’s Journal - listing the “masks work” studies
Goddard’s Journal was among the very first to gather the studies that proved masks work. The author did the work that many governments did not, disproving the lies told about masks.
Goddard’s first video - March 2020
Timings from start of video:
- @ 1:17 Jefferson et al (2011) https://pubmed.ncbi.nlm.nih.gov/21735402 Of the nine case-control studies cited in Goddard's quotation of Jefferson, seven involved healthcare workers and two involved mask wearing by uninfected members of the public, Wu et al (2004) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322931 and Lau et al (2004) @ https://pubmed.ncbi.nlm.nih.gov/15200846
- @ 2:01 Jefferson et al (2008) https://pubmed.ncbi.nlm.nih.gov/18042961
- @ 2:29 MacIntyre (2015) https://pubmed.ncbi.nlm.nih.gov/25858901
- @ 4:09 Hui & Chan (2010) https://pubmed.ncbi.nlm.nih.gov/20674795 and Breban et al (2013) https://pubmed.ncbi.nlm.nih.gov/23831141
- @ 4:21 van Doremalen et al https://www.nejm.org/doi/full/10.1056/NEJMc2004973 and Ong et al (2020) https://jamanetwork.com/journals/jama/fullarticle/2762692
- @ 5:26 Tracht et al (2010) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2818714
- @ 6:58 Cui et al (2019) https://pubmed.ncbi.nlm.nih.gov/31499643/.
- @ 8:22 Tracht et al (2012) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3307882
- @ 9:55 Aiello et al (2012) https://pubmed.ncbi.nlm.nih.gov/22295066
- @ 10:36 Suess et al (2012) https://pubmed.ncbi.nlm.nih.gov/22280120
- @ 11:04 Cowling et al (2009) https://pubmed.ncbi.nlm.nih.gov/19652172
- @ 11:32 Larson et al (2010) https://pubmed.ncbi.nlm.nih.gov/20297744
- @ 12:03 Simmerman et al (2011) https://pubmed.ncbi.nlm.nih.gov/21651736
- @ 12:57 Aiello et al (2012) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3266257
- @ 14:11 MacIntyre (2009) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2662657
- @ 15:45 Foo et al (2006) https://pubmed.ncbi.nlm.nih.gov/17026695
- @ 17:19 DIY facemask https://youtu.be/Pb59qBUNg1o (video)
- @ 18:34 DIY facemask https://youtu.be/Bs-E_R5WWsY (video)
Goddard’s second video - October 2020
This was a follow up to the first, as noted at the start of the video. Timings from start of video:
- @00:30 Wang et al (2020) https://gh.bmj.com/content/5/5/e002794
- @ 01:42 Chan et al (2020) https://academic.oup.com/cid/article/71/16/2139/5848814
- @ 05:28 Chu et al (2020) https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31142-9/fulltext
- @ 10:07 Leung et al (2020) https://www.nature.com/articles/s41591-020-0843-2
- @ 12:03 NHK program on airborne transmission https://youtu.be/vBvFkQizTT4
- @ 12:42 Anfinrud et al (2020) https://www.nejm.org/doi/full/10.1056/NEJMc2007800
- @ 14:02 Fears et al (2020) https://wwwnc.cdc.gov/eid/article/26/9/20-1806_article
- @ 14:33 Lednicky et al (2020) https://www.ijidonline.com/article/S1201-9712(20)30739-6/fulltext
- @ 14:55 Bourouiba (2020) https://jamanetwork.com/journals/jama/fullarticle/2763852
- @ 15:05 Verma et al (2020) https://aip.scitation.org/doi/10.1063/5.0016018
- @ 16:46 Fischer et al (2020) https://advances.sciencemag.org/content/6/36/eabd3083
- @ 19:14 N95 mask-valve leakage. Original: Face Shield or Face Mask to Stop the Spread of COVID-19? by Florida Atlantic University (video)
- @ 20:33 Anti-mask misinformation by retired doctor (no link to the original garbage) See also Politfact debunking (video)
- @ 20:42 That misinformation quickly debunked by Prof Jimenez "Vapor goes thru mask, then condenses" (tweet)
- @ 20:49 Swiss-cheese protection model. Original: RETURN TO WORK AMID COVID-19: A Cleveland Clinic Guide
Scientific studies of masks and respirators
Studies of the use of masks/respirators, thread 🧵. From https://mastodon.social/@jmcrookston/111689874254752367
1. Systematic reviews and meta-analyses of masks and respirators
Summary of the studies listed below
This summary should be accurate but double-check it yourself. Don’t forget about all the limitations of meta-analyses. They have their own intrinsic biases and, of course, are no better than their underlying studies.
The following studies found a statistically significant difference between the data relating tomMasks/respirators and not. This suggests the result (that masks work in the contexts of these trials) was unlikely to be due to random chance.
- Macintyre 2017
- Offeddu 2017. Concluded N95 or surgicalwere effective against clinical respiratory infection.
- Iannone 2020 -
The followng studes did not find a statistically significant difference between the data relating to masks/respirators and not. All we can say is we cannot rule out that these results arose by random chance (at the statistical level selected by the authors). Authors’ comments are noted.
- Smith 2016 - Pooled three trials (Loeb 2009, MacIntyre 2011, MaIcntyre 2013) and found no statistical difference for lab confirmed respiratory infection. Authors noted N95s are better than SM in lab studies.
- Barycka 2020 - meta failed stat but authors noted less illness with N95s.
- Kunstler 2022 - meta N95 vs SM for SARS2. Failed stat but authors noted the direction of effect favoured respirators.
- Chou 2020 -
- Long 2020 -
- Bartoszko & Loeb 2020 - MM vs N95
The studies
2016 Smith, Jeffrey D., Colin C. MacDougall, Jennie Johnstone, Ray A. Copes, Brian Schwartz, and Gary E. Garber. ‘Effectiveness of N95 Respirators versus Surgical Masks in Protecting Health Care Workers from Acute Respiratory Infection: A Systematic Review and Meta-Analysis’. CMAJ: Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne 188, no. 8 (17 May 2016): 567–74. https://doi.org/10.1503/cmaj.150835.
2017 MacIntyre, Chandini Raina, Abrar Ahmad Chughtai, Bayzidur Rahman, Yang Peng, Yi Zhang, Holly Seale, Xiaoli Wang, and Quanyi Wang. ‘The Efficacy of Medical Masks and Respirators against Respiratory Infection in Healthcare Workers’. Influenza and Other Respiratory Viruses 11, no. 6 (2017): 511–17. https://doi.org/10.1111/irv.12474.
2017-11. Offeddu, Vittoria, Chee Fu Yung, Mabel Sheau Fong Low, and Clarence C. Tam. ‘Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis’. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 65, no. 11 (13 November 2017): 1934–42. https://doi.org/10.1093/cid/cix681.
2020-05. Long, Youlin, Tengyue Hu, Liqin Liu, Rui Chen, Qiong Guo, Liu Yang, Yifan Cheng, Jin Huang, and Liang Du. ‘Effectiveness of N95 Respirators versus Surgical Masks against Influenza: A Systematic Review and Meta-Analysis’. Journal of Evidence-Based Medicine 13, no. 2 (May 2020): 93–101. https://doi.org/10.1111/jebm.12381.
2020-07. Bartoszko, Jessica J., Mohammed Abdul Malik Farooqi, Waleed Alhazzani, and Mark Loeb. ‘Medical Masks vs N95 Respirators for Preventing COVID-19 in Healthcare Workers: A Systematic Review and Meta-Analysis of Randomized Trials’. Influenza and Other Respiratory Viruses 14, no. 4 (July 2020): 365–73. https://doi.org/10.1111/irv.12745.
2020-10. Chou, Roger, Tracy Dana, Rebecca Jungbauer, Chandler Weeks, and Marian S. McDonagh. ‘Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings : A Living Rapid Review’. Annals of Internal Medicine 173, no. 7 (6 October 2020): 542–55. https://doi.org/10.7326/M20-3213.
2020 Barycka. ‘Comparative Effectiveness of N95 Respirators and Surgical/Face Masks in Preventing Airborne Infections in the Era of SARS-CoV2 Pandemic: A Meta-Analysis of Randomized Trials’. PloS One 15, no. 12 (2020): e0242901. https://doi.org/10.1371/journal.pone.0242901.
2020 Iannone, Primiano, Greta Castellini, Daniela Coclite, Antonello Napoletano, Alice Josephine Fauci, Laura Iacorossi, Daniela D’Angelo, et al. ‘The Need of Health Policy Perspective to Protect Healthcare Workers during COVID-19 Pandemic. A GRADE Rapid Review on the N95 Respirators Effectiveness’. PloS One 15, no. 6 (2020): e0234025. https://doi.org/10.1371/journal.pone.0234025.
2022-05. Kunstler, Breanne, Skye Newton, Hayley Hill, John Ferguson, Phillipa Hore, Brett G. Mitchell, Kathy Dempsey, et al. ‘P2/N95 Respirators & Surgical Masks to Prevent SARS-CoV-2 Infection: Effectiveness & Adverse Effects’. Infection, Disease & Health 27, no. 2 (May 2022): 81–95. https://doi.org/10.1016/j.idh.2022.01.001.
new
Nanda, Akriti, Ivan Hung, Ava Kwong, Vivian Chi‐Mei Man, Pankaj Roy, Lucy Davies, and Michael Douek. “Efficacy of Surgical Masks or Cloth Masks in the Prevention of Viral Transmission: Systematic Review, Meta‐analysis, and Proposal for Future Trial.” Journal of Evidence-Based Medicine, February 9, 2021, 10.1111/jebm.12424. https://doi.org/10.1111/jebm.12424.
- looked at:
- Aiello 2010
- Aiello 2012
- Barasheed 2014
- Canini 2010
- Cowling 2009
- Cowling 2008
- Larson 2010
- MacIntyre 2009
- MacIntyre 2015
- MacIntyre 2016
- Simmerman 2011
- Suess 2012
- .
-
Results: Fourteen studies were included in this study. One preclinical and 1 observational cohort clinical study found significant benefit of masks in limiting SARS-CoV-2 transmission. Eleven RCTs in a meta-analysis studying other respiratory illnesses found no significant benefit of masks (±hand hygiene) for influenza-like-illness symptoms nor laboratory confirmed viruses. One RCT found a significant benefit of surgical masks compared with cloth masks.” (Nanda et al., 2021, p. 1)
- My comment: Just another “search the lit, select studies, then meta-analyse them”, which one does behind a which adds nothing to the state of knolwedge. Written by doctors, of course, because these sorts of studies are favoured by doctors who cannot do real studies because, as I said, you can do them from behind a desk.
Ollila, Hanna M., Markku Partinen, Jukka Koskela, John Borghi, Riikka Savolainen, Anna Rotkirch, and Liisa T. Laine. “Face Masks to Prevent Transmission of Respiratory Infections: Systematic Review and Meta-Analysis of Randomized Controlled Trials on Face Mask Use.” PLOS ONE 17, no. 12 (December 1, 2022): e0271517. https://doi.org/10.1371/journal.pone.0271517.
SeyedAlinaghi, SeyedAhmad, Amirali Karimi, Amir Masoud Afsahi, Pegah Mirzapour, Sanaz Varshochi, Hengameh Mojdeganlou, Paniz Mojdeganlou, et al. “The Effectiveness of Face Masks in Preventing COVID-19 Transmission: A Systematic Review.” Infectious Disorders Drug Targets, June 1, 2023. https://doi.org/10.2174/1871526523666230601090905.
- “Introduction: Since the beginning of the COVID-19 pandemic, face masks have been among the cornerstones of COVID-19 prevention. Therefore, evaluating their preventive effects against COVID-19 is crucial. This review aimed to systematically search for the systematic review articles that explored the role of various types of face masks in preventing COVID-19. Methods: We browsed the keywords of this study in the online databases of Scopus, Web of Science, PubMed, and Cochrane on 10th January 2023 and retrieved all the relevant systematic review articles. The records were downloaded into an Endnote file, and the duplicates were removed. A two-step screening process consisting of title/abstract and full-text screenings was conducted to select the most relevant articles. To ensure the validity and reliability of the results, this study adhered to the PRISMA protocol. Results: A total of 28 systematic reviews were included in this review. Most studies found that face masks are beneficial against viral respiratory infections, such as COVID-19. Different types of masks were evaluated in included studies. It appeared that mask efficacy depends on the material, layers, fitting on the face and user compliance. N 95 respirator had maximum efficacy, especially when used continuously. Conclusion: Face masks have a beneficial effect against COVID-19. Home masks are less protective than surgical masks or N95 personal breathing masks. Besides, the use of masks may elicit a false sense of security in people, which may lead to poor hand hygiene and violation of social distancing. Therefore, the necessary training should be provided to the public to increase awareness and encourage the right practice of using the mask, emphasizing the preventive effects of washing hands, social distancing, and using a face mask against COVID-19.”
Boulos, Leah, Janet A. Curran, Allyson Gallant, Helen Wong, Catherine Johnson, Alannah Delahunty-Pike, Lynora Saxinger, et al. “Effectiveness of Face Masks for Reducing Transmission of SARS-CoV-2: A Rapid Systematic Review.” Philosophical Transactions. Series A, Mathematical, Physical, and Engineering Sciences 381, no. 2257 (n.d.): 20230133. https://doi.org/10.1098/rsta.2023.0133.
- I would not trust this paper.
MacIntyre, C. Raina, and Abrar Ahmad Chughtai. “A Rapid Systematic Review of the Efficacy of Face Masks and Respirators against Coronaviruses and Other Respiratory Transmissible Viruses for the Community, Healthcare Workers and Sick Patients.” International Journal of Nursing Studies 108 (August 2020): 103629. https://doi.org/10.1016/j.ijnurstu.2020.103629.
2. Narrative reviews (summaries of studies)
Schünemann, Holger J., Elie A. Akl, Roger Chou, Derek K. Chu, Mark Loeb, Tamara Lotfi, Reem A. Mustafa, et al. ‘Use of Facemasks during the COVID-19 Pandemic’. The Lancet. Respiratory Medicine 8, no. 10 (October 2020): 954–55. https://doi.org/10.1016/S2213-2600(20)30352-0.
Regli, A., A. Sommerfield, and B. S. von Ungern-Sternberg. “The Role of Fit Testing N95/FFP2/FFP3 Masks: A Narrative Review.” Anaesthesia 76, no. 1 (January 2021): 91–100. https://doi.org/10.1111/anae.15261.
Howard, Jeremy, Austin Huang, Zhiyuan Li, Zeynep Tufekci, Vladimir Zdimal, Helene-Mari van der Westhuizen, Arne von Delft, et al. “An Evidence Review of Face Masks against COVID-19.” Proceedings of the National Academy of Sciences 118, no. 4 (January 26, 2021). https://doi.org/10.1073/pnas.2014564118.
3. Studies (actual studies, so excludes meta-analyses)
Radonovich, Lewis J., Michael S. Simberkoff, Mary T. Bessesen, Alexandria C. Brown, Derek A. T. Cummings, Charlotte A. Gaydos, Jenna G. Los, et al. ‘N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial’. JAMA 322, no. 9 (3 September 2019): 824–33. https://doi.org/10.1001/jama.2019.11645.
Ueki, Hiroshi, Yuri Furusawa, Kiyoko Iwatsuki-Horimoto, Masaki Imai, Hiroki Kabata, Hidekazu Nishimura, and Yoshihiro Kawaoka. “Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2.” mSphere, October 21, 2020. https://doi.org/10.1128/mSphere.00637-20.
“The N95 mask had the highest protective efficacy (approximately 80% to 90% reduction) of the various masks examined; however, infectious virus penetration was measurable even when the N95 mask was completely fitted to the face with adhesive tape (Fig. 2B). In contrast, when a mask was attached to the mannequin that released virus, cotton and surgical masks blocked more than 50% of the virus transmission, whereas the N95 mask showed considerable protective efficacy (Fig. 2C). There was a synergistic effect when both the virus receiver and virus spreader wore masks (cotton masks or surgical masks) to prevent the transmission of infective droplets/aerosols (Fig. 2D and E).” ([Ueki et al., 2020, p. 3]
Ferris, Mark, Rebecca Ferris, Chris Workman, Eoin O’Connor, David A Enoch, Emma Goldesgeyme, Natalie Quinnell, et al. “Efficacy of FFP3 Respirators for Prevention of SARS-CoV-2 Infection in Healthcare Workers.” Edited by Jos W Van der Meer, Sarah Logan, and Stephanie Evans. eLife 10 (November 16, 2021): e71131. https://doi.org/10.7554/eLife.71131.
“Results: Whilst using FRSMs, HCWs working on red wards faced an approximately 31-fold (and at least fivefold) increased risk of direct, ward-based infection. Conversely, after changing to FFP3 respirators, this risk was significantly reduced (52–100% protection). Conclusions: FFP3 respirators may therefore provide more effective protection than FRSMs for HCWs caring for patients with COVID-19, whether or not AGPs are undertaken.” ([Ferris et al., 2021, p. 1]
- After adjustment for under-testing, mask mandates emerged as highly effective. Community masking saved substantial numbers of lives, and prevented economic costs, during the SARS-CoV-2 pandemic in Ontario, Canada.
https://academic.oup.com/pnasnexus/advance-article/doi/10.1093/pnasnexus/pgae065/7606553
2. Studies of masks as source control
Lai, Jianyu, Kristen K. Coleman, S.-H. Sheldon Tai, Jennifer German, Filbert Hong, Barbara Albert, Yi Esparza, et al. “Relative Efficacy of Masks and Respirators as Source Control for Viral Aerosol Shedding from People Infected with SARS-CoV-2: A Controlled Human Exhaled Breath Aerosol Experimental Study.” eBioMedicine 104 (June 1, 2024). https://doi.org/10.1016/j.ebiom.2024.105157.
Verma, Siddhartha, Manhar Dhanak, and John Frankenfield. “Visualizing the Effectiveness of Face Masks in Obstructing Respiratory Jets.” Physics of Fluids 32, no. 6 (June 1, 2020): 061708. https://doi.org/10.1063/5.0016018.
Epidemiological studies
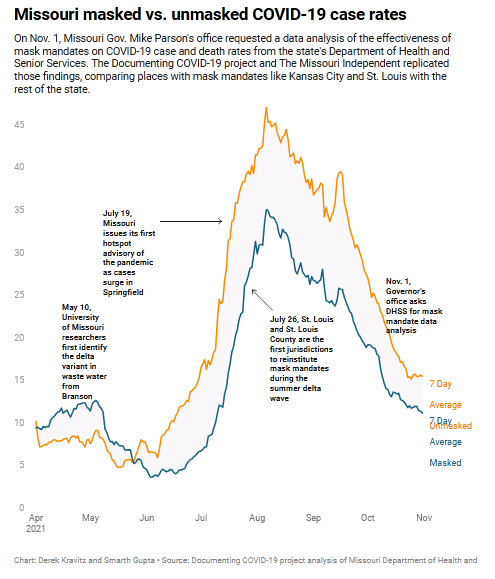
2021 Dec. Missouri health department found mask mandates work, but didn’t make findings public. “Jurisdictions with mask mandates averaged 15.8 cases per day for every 100,000 residents, compared to 21.7 in unmasked communities. https://archive.ph/EK5tt.
Loeb study (2009) and its criticisms
Loeb, Mark, Nancy Dafoe, James Mahony, Michael John, Alicia Sarabia, Verne Glavin, Richard Webby, et al. “Surgical Mask vs N95 Respirator for Preventing Influenza among Health Care Workers: A Randomized Trial.” JAMA 302, no. 17 (November 4, 2009): 1865–71. https://doi.org/10.1001/jama.2009.1466.
criticisms:
Bitar, Roger. “Surgical Masks vs N95 Respirators for Preventing Influenza.” JAMA 303, no. 10 (March 10, 2010): 937; author reply 938-939. https://doi.org/10.1001/jama.2010.193.
Clynes, Neville. “Surgical Masks vs N95 Respirators for Preventing Influenza.” JAMA 303, no. 10 (March 10, 2010): 937–38; author reply 938-939. https://doi.org/10.1001/jama.2010.194.
Finkelstein, Yaron, Tal Schechter, and Stephen B. Freedman. “Surgical Masks vs N95 Respirators for Preventing Influenza.” JAMA 303, no. 10 (March 10, 2010): 938; author reply 938-939. https://doi.org/10.1001/jama.2010.195.
Palen, Ted E., and Kate G. Felix. “Surgical Masks vs N95 Respirators for Preventing Influenza.” JAMA 303, no. 10 (March 10, 2010): 937; author reply 938-939. https://doi.org/10.1001/jama.2010.192.
Anti-Masker activities
Anti-masker groups are motivated by politics, hatred of your group/country, bad science, and more. They link to things they claim can prove their case, but which are always based on bad science or logic.
Their bogus talking points:
- “just search for it, I don’t have to give you links to studies”
- “masks starve your oxygen” - they do not
- “Country X or state Y doesn’t have masks, and they’re better than your country”. Ask them what they think about Taiwan or South Korea who’ve performed among the best (with masks), and they get all racist or suggest it is faked.
Raina MacIntyre’s work in particular
Study ‘MacIntyre et al, 2015’, figures quite a lot as an anti-masker “truth”. Goddard’s Journal went into this study above. Meanwhile, Raina C MacIntyre is disgusted with mis-representation by anti-masker groups. She has published more in the last eighteen months to further indicate her science that masks actually work and that we should wear them:
- June 24, 2020; Prof Raina MacIntyre in a Guardian article: "People are still kind of stuck in that mindset of hand sanitiser and washing your hands, when actually the message we need to be getting out there is it’s the air you breathe … and you should wear masks"
- May 12, 2021; Prof Raina MacIntyre in a TheConversation article: "in further evidence the droplet theory is false, we showed that even for infections believed to be spread by droplets, a N95 respirator protects better than a surgical mask. In fact airborne precautions are needed for most respiratory infections."
- January 21, 2021; Prof Raina MacIntyre in Croakey Health Media eZine: "The lack of experts on respiratory transmissible infection or aerosol science at the table meant that much of 2020 was spent on promotion of hygiene theatre, actively discouraging mask use and a resulting low awareness among the general public of the importance of ventilation and masks in reducing their personal risk."
- December 20, 2020; Prof Raina MacIntyre in the Sydney Morning Herald: “Mandating masks across greater Sydney will make a difference”
- December 17, 2020; Prof Raina MacIntyre in the Sydney Morning Herald: “Until we address airborne transmission, we fail to address masks and ventilation and keep peddling the myth that washing hands and wiping surfaces is enough. We need universal masking in closed public spaces”
- October 12, 2020; Prof Raina MacIntyre in the Sydney Morning Herald: “Mandating masks in public places would reduce the risk of transmission from asymptomatic or mildly symptomatic people, protect well people, and enable greater freedom of movement.”
- September 29, 2020; Prof Raina MacIntyre in BMJ Opinion: Cloth masks should be washed appropriately everyday.
- July 4, 2020, Prof Raina MacIntyre in the Sydney Morning Herald: “Face masks have not been recommended actively, although would likely help control the epidemic in Victoria. There is increasing evidence that spread of SARS-CoV-2 is as much due to the air we breathe as it is to what we touch or who coughs in our face. This, plus asymptomatic infection, is a reason why physical distancing and masks are a good idea.”
- June 27, 2020, Prof Raina MacIntyre in The Lancet: Physical distancing, face masks, and eye protection for prevention of COVID-19
- April 21, 2021, The Impact of Universal Mask Use on SARS-COV-2 in Victoria, Australia on the Epidemic Trajectory of COVID-19